The inability to waken differentiates coma from sleep. Levels of unconsciousness and unresponsiveness vary, depending on how much of the brain is functioning.
A coma is a medical emergency that requires rapid action to preserve life and brain function. Generally, doctors will order a series of blood tests and imaging scans to try to find out what the cause of the coma is. Determining the cause usually decides what type of treatment to apply.
Coma may occur for various reasons, such as intoxication, CNS (central nervous system) diseases, a serious injury, and hypoxia (oxygen deprivation). Coma can be induced deliberately with pharmaceutical agents – perhaps in order to protect the patient from intense pain during a healing process, or to preserve higher brain function following another form of brain trauma.
Comas generally do not last for more than a few weeks. A patient whose state does not change after an extended period is often reclassified as being in a persistent vegetative state. Unfortunately, those in a persistent vegetative state for over twelve months rarely wake up.
According to Medilexicon’s medical dictionary:
Coma is “A state of profound unconsciousness from which one cannot be roused; may be due to the action of an ingested toxic substance or of one formed in the body, to trauma, or to disease.”
The English medical word “coma” comes from the Ancient Greek word Koma, meaning “deep sleep”.
What are the signs and symptoms of a coma?
A symptom is something the patient feels and reports, while a sign is something other people, such as the doctor detect. For example, pain may be a symptom while a rash may be a sign. As a comatose patient does not communicate, there are only signs:
* Closed eyes
* Limbs do not respond, except for reflex movements
* There is no response to painful stimuli, except for reflex movements
The severity and duration of signs and symptoms that led up to the loss of consciousness may vary and depend on the underlying cause. For example, worsening hypoglycemia (low blood sugar) or hypercapnia (higher blood CO2 levels) will cause mild agitation at first, eventually there will be obtundation (less than full mental capacity), stupor and finally loss of consciousness. On the other hand, coma caused by a severe injury to the brain or a subarachnoid hemorrhage will occur instantaneously. Doctors are especially interested in what occurred leading up to the coma, because that helps them determine what the underlying cause was and what treatment to apply.
When doctors initially assess a coma, they will typically try to gauge the level of consciousness by spontaneously exhibited actions. The AVPU scale is an example; the abbreviation stands for
Alert
Vocal stimuli
Painful stimuli
Unconscious
More elaborate scales also exist, such as the Glasgow coma scale (see further down this page). Patients with deep unconsciousness are assessed for risk of asphyxiation – if it is high some type of device may be used to secure the airways, such as an oropharyngeal airway, nasopharyngeal airway or endotracheal tube.
What are the possible causes of a coma?
A coma can have several possible causes, including:
* Diabetes – if the blood sugar levels of the diabetes patient rise too much they will have hyperglycemia, the opposite is hypoglycemia (blood sugar levels are too low). Sustained periods of hyperglycemia or hypoglycemia can result in coma.
* Hypoxia (lack of oxygen) – a person who nearly drowned may not awaken because of a shortage of blood (which carries oxygen) to the brain. The same may occur to somebody who is resuscitated after a heart attack.
* Infections – those which cause inflammation of the brain, spinal cord or tissues surrounded the brain can result in coma if symptoms are severe enough. Examples include encephalitis or meningitis.
* Stroke – a condition where a blood clot or ruptured artery or blood vessel interrupts blood flow to an area of the brain. A lack of oxygen and glucose (sugar) flowing to the brain leads to the death of brain cells and brain damage, often resulting in impairment in speech, movement, and memory – and sometimes coma.
* Toxins and drug overdoses – exposure to carbon monoxide can result in brain damage and coma, as can some drug overdoses.
* Traumatic brain injuries – these include injuries from vehicle accidents and violent attacks. They are the most common cause of comas.
Diagnosing comatose patients
The health care team cannot glean information from the patient and have to rely on signs (physical clues), as well as information from friends, family, police and witnesses. The following questions are commonly asked:
* “Did the coma come on rapidly or gradually?”
* “Did the patient experience any vision problems, dizziness, stupor or numbness before the coma?”
* “Does the patient have diabetes, any history of seizures or strokes – or any other conditions or diseases?”
* “What medications has the patient been taking/given?”
Physical tests – the aim is to check the patient’s reflexes, whether or not he/she responds to pain, and pupil size. This may involve squirting very cold or warm water into the ear canals. These tests will trigger varying reflexive eye movements – the type of response varies according to the cause of the coma.
Blood tests – these will be taken to determine:
* Blood count
* Carbon monoxide poisoning
* Drug overdose
* Electrolytes
* Glucose
* Liver function
Lumbar puncture (spinal tap) – this can determine whether there is an infection. The doctor inserts a needle into the patient’s spinal canal, measures pressure and extracts fluid.
Imaging scans of the brain – these will help determine whether there is any brain injury/damage, and where. Examples include:
* CT (computed tomography) scan – also known as a CAT (Computer Axial Tomography) scan. It is a medical imaging method that employs tomography. Tomography is the process of generating a two-dimensional image of a slice or section through a 3-dimensional object (a tomogram). The medical device is called a CTG scanner; it is a large machine and uses X-rays. It used to be called an EMI scan, because it was developed by the company EMI.
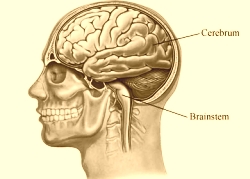
* MRI (magnetic resonance imaging) scan – an MRI machine uses a magnetic field and radio waves to create detailed images of the body, which in this case would be the brain. Most MRI machines look like a long tube, with a large magnet present in the circular area. When beginning the process of taking an MRI, the patient is laid down on a table. Then depending on where the MRI needs to be taken, the technician slides a coil to the specific area being imaged. The coil is the part of the machine that receives the MR signal. MRI scans are good for examining the brainstem and deep brain structures. The doctor may inject a special dye which shows up on the scans and distinguishes healthy tissue from damaged tissue.
* EEG (electroencephalography) – the device measures the electrical activity within the brain. Electrodes are placed on the patient’s scalp; they pick up electrical impulses that occur in the brain. These impulses are recorded on the EEG device. An EEG can tell whether the patient is having non-convulsive seizures.
Glasgow Coma Scale
Doctors often use the Glasgow Coma Scale (GCS) before deciding whether to use a CT scan. The GCS is a way for doctors and nurses to assess the severity of brain damage following a head injury. It scores patients according to verbal responses, motor responses (physical reflexes), and how easily they can open their eyes.
* Eyes – Glasgow Coma Scale
Score of 1 – does not open eyes.
Score of 2 – opens eyes in response to painful stimuli (when given pain).
Score of 3 – opens eyes in response to voice.
Score of 4 – opens eyes spontaneously.
* Verbal – Glasgow Coma Scale
Score of 1 – makes no sound.
Score of 2 – incomprehensible sounds (mumbles).
Score of 3 – utters inappropriate words.
Score of 4 – confused, disorientated.
Score of 5 – oriented, chats normally.
* Motor (physical reflexes) – Glasgow Coma Scale
Score of 1 – makes no movements.
Score of 2 – extension to painful stimuli (straightens limb when given pain).
Score of 3 – abnormal flexion to painful stimuli (moves in a strange way when given pain).
Score of 4 – flexion/withdrawal to painful stimuli (moves away when given pain).
Score of 5 – localizes painful stimuli (can pinpoint where pain is).
Score of 6 – obeys commands.
* Brain injury will be classified in the Glasgow Coma Scale as:
Coma = a score of 8 or less.
Moderate = a score of 9 to 12.
Minor = a score of 13 or more.
What are the treatment options for a coma?
A coma is a serious medical emergency. The medical team’s first priority is the immediate survival of the patient, which typically includes maintaining respiration and circulation (of blood). In some cases the patient may require assistance in breathing, as well as receiving fluids and blood.
Even before blood test results come in, the medical team may administer glucose or antibiotics, in case the patient is in diabetic shock or has a brain infection.
The main determinant of the type of treatment is the underlying cause of the coma, for example kidney failure, liver disease, diabetes, poisoning, etc.
If there is brain swelling surgery may be needed to relieve the pressure.
If the cause of the coma can be successfully treated there is an excellent chance the patient will eventually awaken with no permanent damage. Unfortunately, if brain damage is severe, they may have long-term problems and disabilities, or might never wake up.
Written by Christian Nordqvist