 laboratory reporting of newly diagnosed hepatitis C infections in England increased in 2008 by 6% compared to 2007, with 8,196 new cases reported in 2008.
laboratory reporting of newly diagnosed hepatitis C infections in England increased in 2008 by 6% compared to 2007, with 8,196 new cases reported in 2008.
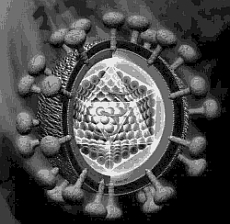
Hepatitis C is a viral infection which causes swelling or inflammation of the liver. It is transmitted when the blood of an infected person mixes with a recipient’s blood, such as via injecting drug use and the sharing of needles. Because hepatitis C infection is predominantly asymptomatic in the early years, many individuals remain undiagnosed until the disease has progressed. If the infection is diagnosed in the early stages, treatment can be offered that can clear the infection in more than half of those treated. However, some infections remain undiagnosed until end-stage liver disease is reached, when a transplant becomes the only real option.
It is estimated that currently around 185,000 individuals in the UK are chronically infected with hepatitis C (142,000 in England & Wales, 39,000 in Scotland and 4,000 in Northern Ireland); these individuals are at risk of developing serious liver disease.
Predictions from the HPA indicate that the future burden of this disease on the health service will be substantial if awareness, diagnosis and treatment do not increase. This can already be seen in national mortality figures, hospital admissions and transplant data, which all show that hepatitis C related serious liver disease is continuing to increase year-on-year.
The increase in newly diagnosed cases may be attributable in part to the public information campaigns and the subsequent increase in awareness which has encouraged more people to come forward and get tested. Awareness of hepatitis C may be increasing in the general population, as well as in key risk groups.
 Dr Helen Harris, a hepatitis C expert from the Health Protection Agency, said: “Too many people with hepatitis C are still undiagnosed. It is critical that awareness campaigns are sustained and enhanced if more people at risk of this infection are to be tested and treated.
Dr Helen Harris, a hepatitis C expert from the Health Protection Agency, said: “Too many people with hepatitis C are still undiagnosed. It is critical that awareness campaigns are sustained and enhanced if more people at risk of this infection are to be tested and treated.
“Liver disease is largely preventable and yet it continues to rise unlike other major causes of death in the UK such as cancer, heart disease and stroke. Tackling undiagnosed hepatitis C infections by increasing awareness and encouraging testing could have a major impact on the number of people suffering needlessly from liver disease in the future.”
Recent campaigns to raise awareness of hepatitis C have included the ‘Get tested, Get treated’ campaign launched this year to target former injecting drug users together with a campaign targeting the South Asian community, who are at increased risk of infection and who may have acquired their infections via other routes. Other work on a national level to tackle hepatitis C and the other causes of liver disease has included creating the new position of National Clinical Director, who will lead on the development of a national liver strategy.
The work of the Health Protection Agency includes monitoring trends in hepatitis C at a national level and working with other agencies through a network of local leads to improve services for the prevention, diagnosis and treatment of hepatitis.
Currently, the greatest risk of contracting hepatitis in the UK is through sharing equipment for injecting drugs. Sharing injecting equipment, even on a one-off basis, or a long time ago (as many people remain asymptomatic for years), could place an individual at risk of hepatitis C.
Notes
1. ‘Hepatitis C in the UK – 2009 Report’ summarises current knowledge about hepatitis C and the action being taken to tackle the infection. To see a full copy of the report, visit: https://www.hpa.org.uk/hepC2009
2. Anyone who thinks they might have been put at risk of infection should contact their GP or call the Hepatitis C Information Line on 0800 451 451 for confidential information and advice, or visit https://www.nhs.uk/hepc.
3. General information about hepatitis C is available at the Health Protection Agency website.
4. Hepatitis is the swelling or inflammation of the liver. The most common causes of hepatitis are viral infections, such as hepatitis C. Some of the other main causes of liver disease include alcohol and obesity.
5. Laboratory reports with risk factor information suggest that more than 90% of laboratory confirmed cases of hepatitis C between 1996 and 2008 were acquired via injecting drug use. 68% of reported cases are among men and 50% between the ages of 25 and 39 years.
6. Other groups at risk of infection include those who have received a blood transfusion before September 1991 or blood products before 1986 in the UK, as well as those who originate from countries where hepatitis C is endemic. Less common ways to become infected include: – from infected mother to baby before or during birth
– having medical and dental treatment abroad, where unsterile equipment may have been used
– tattooing or body piercing where unsterile equipment may have been used
– sharing razors or toothbrushes that may have been contaminated with blood from someone who is infected
Source
Health Protection Agency
