A report published in The Lancet in November stated that Human Embryonic Stem Cells (hESCs) could be used to treat seriously burnt patients by providing temporary skin substitutes.
According to the normal protocol, seriously burnt patients are treated through cell therapy, which involves using the patients own skin cells (keratinocytes) to recover from their injuries. A timeframe no less than three weeks is required to culture these cells in a laboratory and later use them to replace skin of a burnt patient. To overcome this time lag that could also cause dehydration and infection, patients have routinely been treated using decellularised skin from deceased persons to cover wounds. However, its availability is limited and being a foreign body, donor cells are often rejected by the patient.
To circumvent this problem, scientists of this study pharmacologically seeded hESCs onto feeder cells over a period of 40 days. This method employs biological steps that lead to the formation of epidermis during embryonic development, finally forming a keratinocyte linage. Once placed on an artificial matrix, this linage was able to develop a layer of the skin. In 12 weeks, after grafting it onto five mice, the skin layer that came from human embryonic stem cells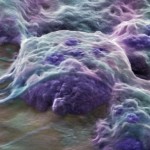 had a structure that was “consistent” with human skin.
had a structure that was “consistent” with human skin.
The authors explain: “We have shown that keratinocytes can be derived from hESCs. Growing human epidermis from hESCs could have clinical relevance as an unlimited resource for temporary skin replacement in patients with large burns awaiting autologous grafts.”
Research is still underway to weigh out the possibility of using this method to develop permanent skin grafts.
In a comment accompanying the article, Holger Schluter, PhD, and Pritinder Kaur, PhD, of the Epithelial Stem Cell Biology Laboratory in Melbourne, Australia, say the latest study “takes research into regenerative skin stem cells to the next level” and “suggests” that cells made from human embryonic stem cells could be transplanted onto burn patients who are awaiting the growth of their own cells.
Article by Snigdha Taduri for Biomed-ME
