New Guidelines Recommend Pap Smears Every Two Years To Reduce Risk From Unnecessary Treatment
The new guidelines from the American College of Obstetricians and Gynaecologists or ACOG recommend starting cervical cancer screening at 21 years and extend routine pap smears to once in two years instead of an annual exam for those younger than 30, and once every three years for those over 30. On the other hand, women with HIV, other immune-weakening conditions or previous cervical abnormalities may need more frequent screening.
Amidst widespread concerns that the government is trying to cut health costs by limiting cancer screening for women, the new guidelines stem from scientific research that states that frequent testing leads to overtreatment, which in turn impairs a woman’s chances of carrying her baby full term.
According to Dr. Jennifer Milosavijevic, a specialist in obstetrics and gynaecology at Henry Ford Health System in Detroit and a supporter of the guidelines, “Preterm delivery has become a huge problem in the United States that has potential serious consequences for the unborn foetus. These new guidelines will allow us to avoid doing unnecessary procedures on the sexually active adolescent female.” 
Prior recommendations of cervical screening required women to be screened three years after they first became sexually active. Dr. Thomas Herzog of Columbia University in New York, who is chairman of an ACOG subcommittee on gynaecologic cancers said, “We were over-diagnosing and over-treating adolescents and very young women and screening earlier than age 21 causes more harm than benefit.”
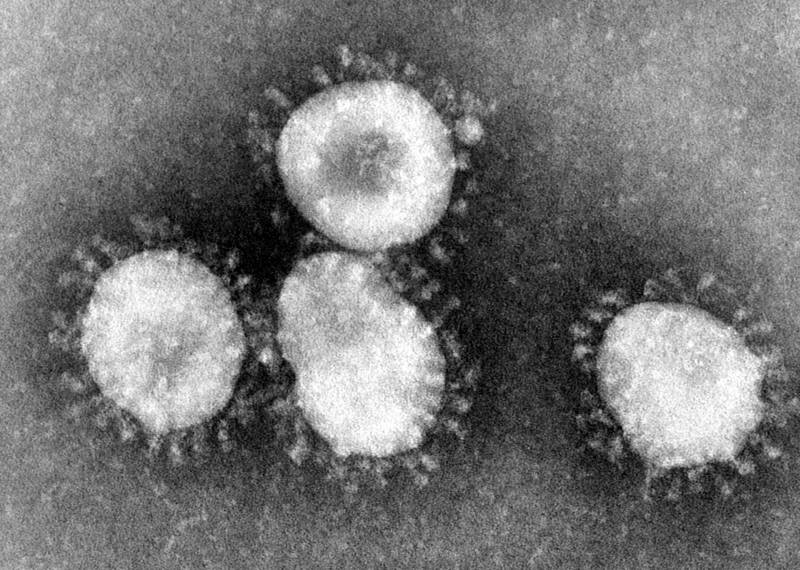
Cervical cancer is a slow growing cancer caused by Human Papilloma Virus (HPV), the sexually transmitted virus that causes precancerous abnormalities of the cervix. It takes years of HPV infection to actually manifest into cancer and for this reason, changing the frequency of pap smear testing doesn’t increase the risk of cervical cancers being missed. On the contrary, deaths from cervical cancer occur due to either infrequent screening or no screening at all.
According to Dr. Len Lichtenfeld, deputy chief medical officer of the American Cancer Society, there is a lot more agreement about the science of cervical cancer screening.
HPV, the most common sexually transmitted disease in the world, affects about 20 million Americans currently. Pap smears can spot pre cancerous changes occurring in the cervical region much before it turns fully cancerous, thus greatly reducing the number of such cases in the last thirty years.